Hip dysplasia or Developmental Dysplasia of the Hip (DDH) is a condition characterised by the abnormal growth of the hip, manifesting general instability or looseness of the hip joint.
Initially, Congenital Hip Dysplasia was the most common term used to describe this condition, since it primarily affects patients who are born with an abnormal hip joint that can result in hip dysplasia. However this condition not only affect newborns but can also occur at any time of hip development. For this reason, Developmental Dysplasia of the Hip (DDH) is considered the most accurate term to describe this condition.
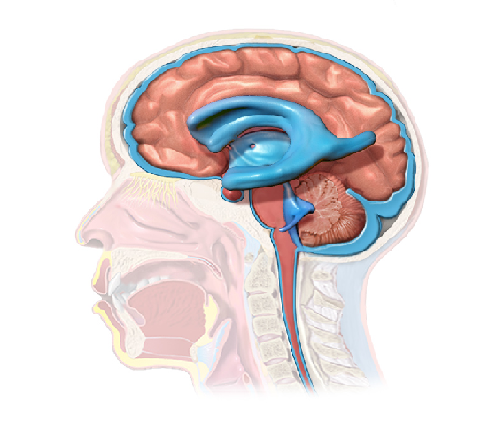
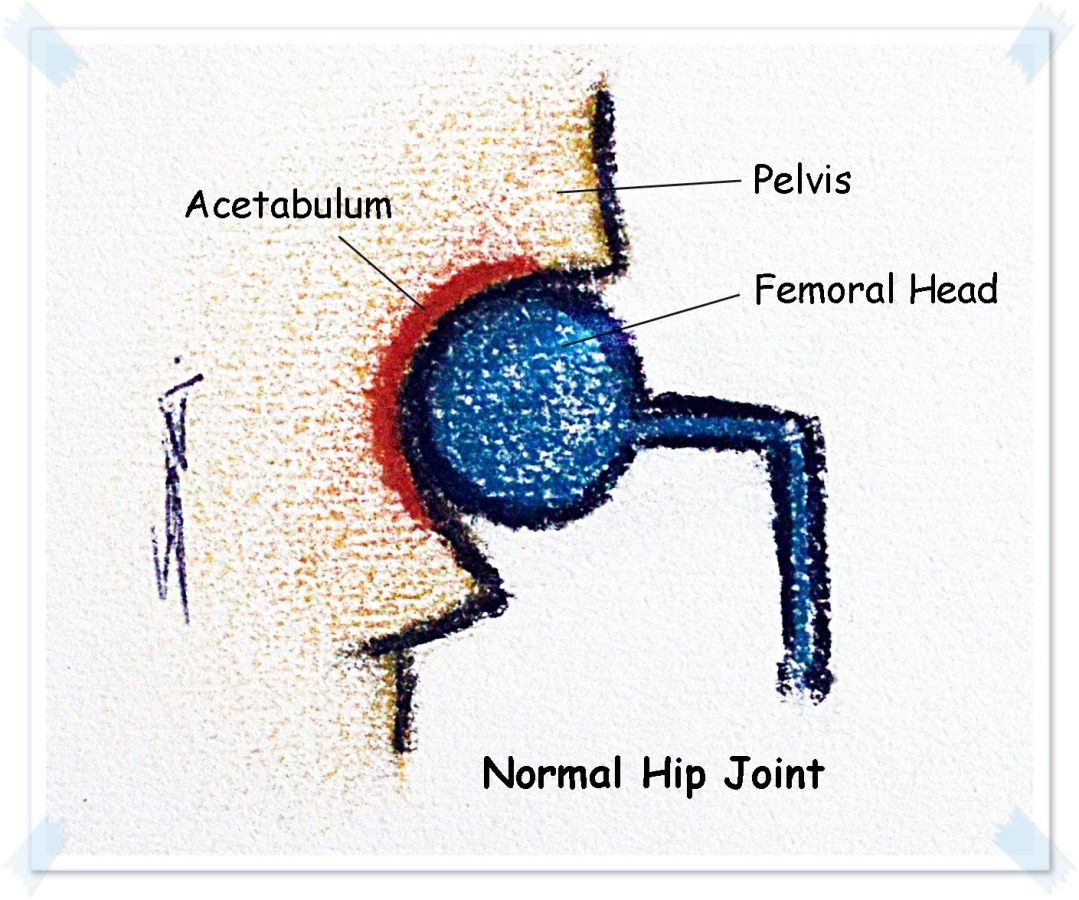
Anatomy review:
The hip is the articulation of the pelvis with the femur, considered as a “ball-and-socket” joint, in which the ball is the femoral head and the socket is the acetabulum. Other important structures of the hip joint are the ligaments and the capsule that hold the joint together .
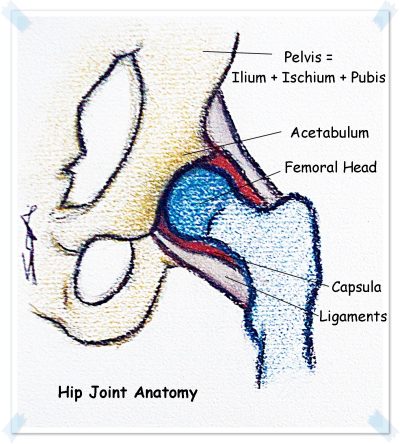
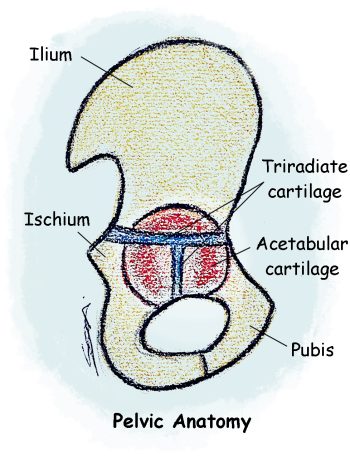
The acetabulum is the structure of the pelvis that comes in contact with the femoral head and is composed by the acetabular portion of the three pelvic bones: ilium, ischium, and pubis.
Important fact: At birth those pelvic bones are separated by a Y-shaped cartilage, known as triradiate cartilage, but during the puberty the cartilage begins to narrow and it becomes completly ossified around age of 15 to 18, forming the innominate bone. Because it ossifies, it is crucial that during that process the femoral head is positioned in a correct place for a normal development of the acetabulum, as the ball and socket act as molds to each other.
Diagnosis: If an abnormal growth of the hip occur and the femoral head is not correctly in place, an earlier DDH diagnose and treatment is essential for a better outcome. Some of the following signs and tests are used to assess the hip and diagnose this condition.
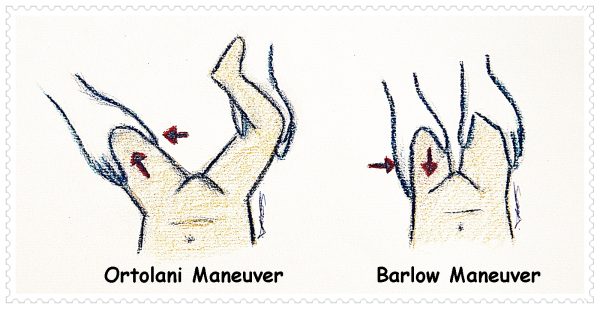
- Ortolani maneuver – a gentle upward force is applied while the hip is abducted; used in children 3 months or yonger;
- Barlow maneuver – a gentle downward force is applied while the hip is adducted used in children 3 months or yonger;
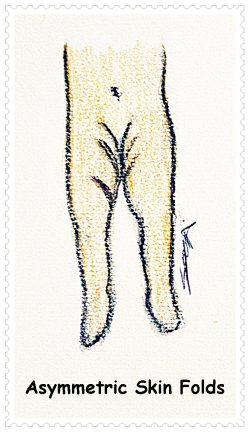
- Asymmetric skinfolds in the upper thigh or leg length inequality; only visible if unilateral hip dysplasia;
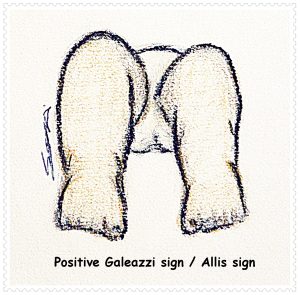
- Positive Galeazzi sign / Allis sign– when the knees are at different heights, with patient in supine position and hips and knees flexed; only visible if unilateral hip dysplasia;
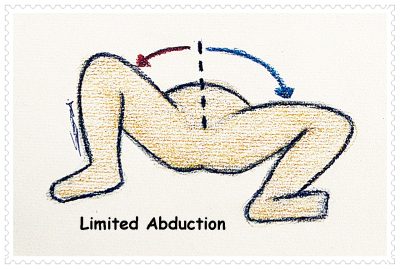
- Limited hip abduction – side affected has limited hip abduction; if bilateral hip dislocation, this constitutes an important diagnostic sign, as the Galeazzi test is not effective in these situations, since the lengths of the children’s legs are the same;
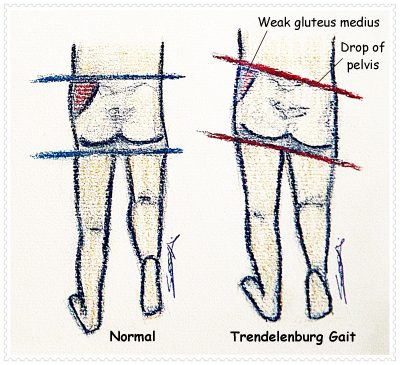
- Trendelenburg’s symptom / Trendelenburg gait – when the child walks and a limp on the affected side is noted.
There are different types of hip dysplasia depending on its severity:
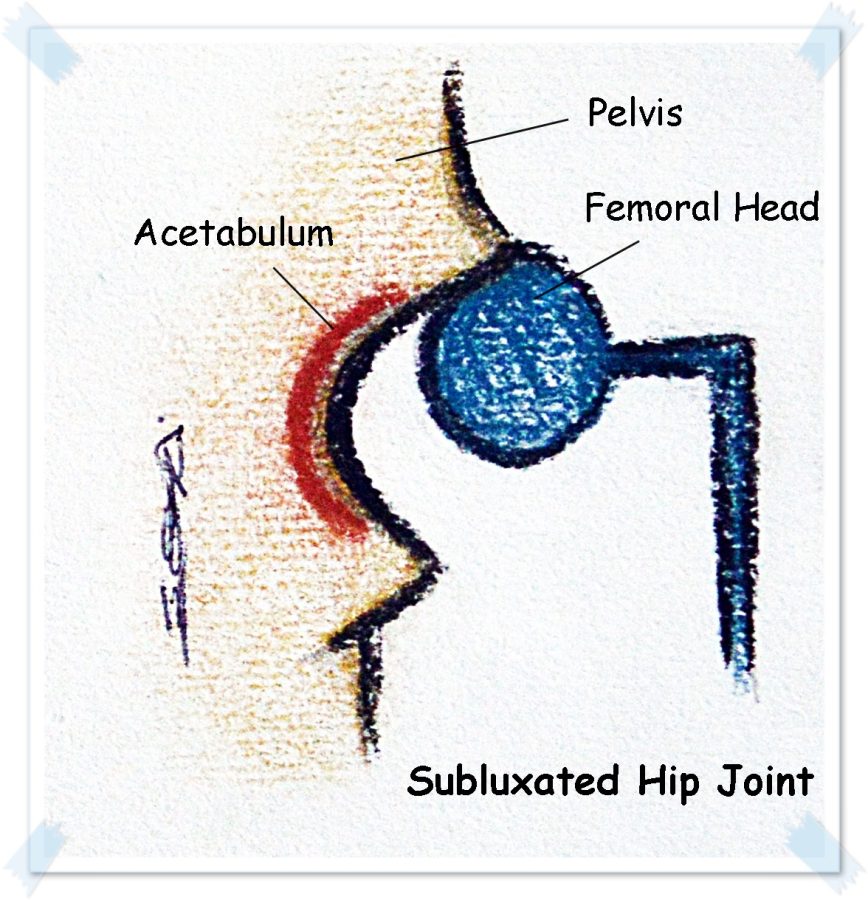
- Subluxation – when the femoral head is not placed in a normal position but still makes contact with a portion of the acetabulum (incomplete contact);
- Unstable / Dislocatable hip – when the femural head is in the acetabulum but may be subluxated or dislocated by passive manipulation during a physical exam;
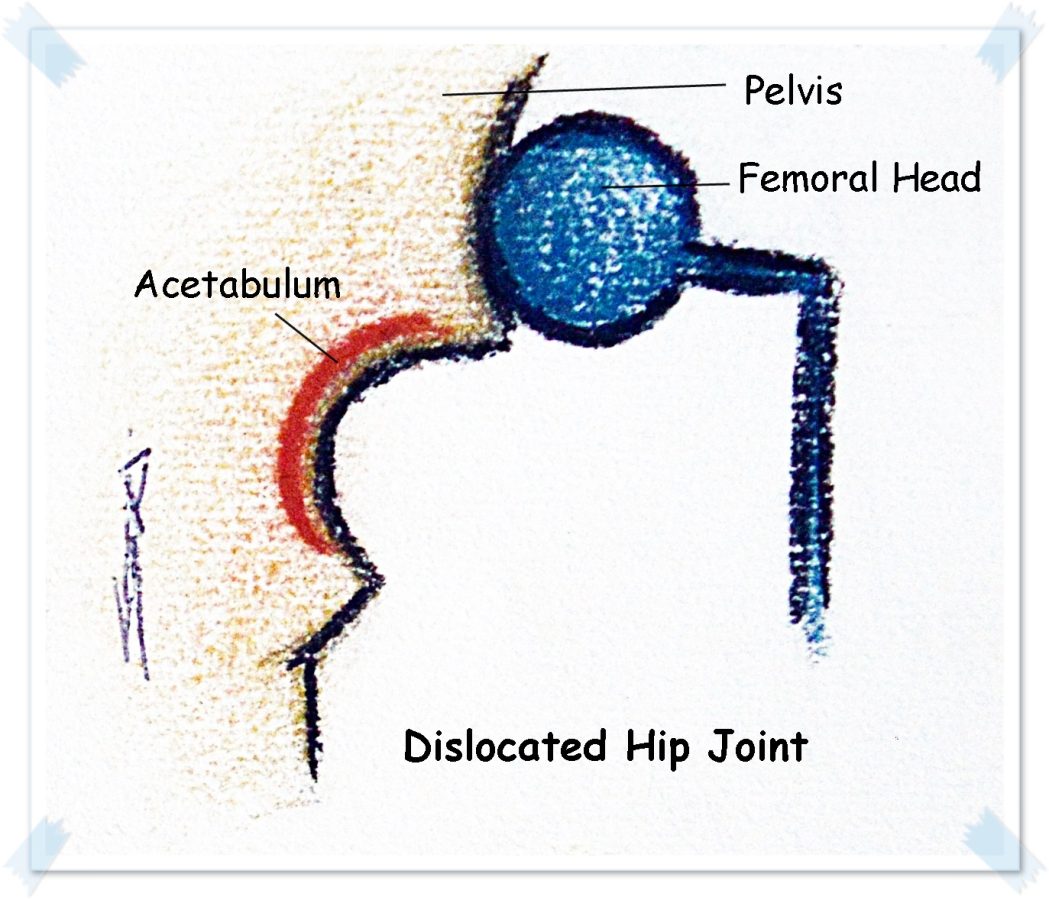
- Dislocation/ Luxation – there is a total loss of contact between the femoral head and the acetabulum.
DDH Treatments:
The treatments available depend on severity of hip dysplasia and on patient’s age. And in some cases, multiple approaches and surgeries are required to treat this condition.
A) Spontaneous correction with no treatment – for newborns with subluxation of hip; if condition persist after 2 weeks of age proceed for treatment;
B) Immobilization in a brace or harness device (usually Pavlik harness) – for babies from birth to 6 months with instable hip upon examination; if Pavlik harness is not effective the use of a firmer device may be required.

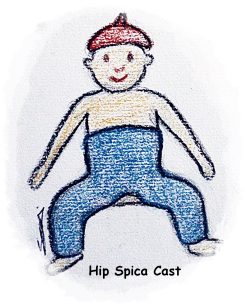
C) Closed reduction + hip spica casting +/- traction before surgery – usually for children older than 6 months to 2 years who present dislocatable or dislocated hip; or for younger children whose previous treatment was not effective; skin traction may be required before surgery to prepare soft tissues around hip joint for the future changes in bone positioning; closed reduction includes: Arthrogram, Adductor Tenotomy, Hip Reduction (by physical manipulation under x-ray) and Spica casting.
D) Open reduction +/- casting – for children older than 2 years, or younger if previous treatment was not effective; surgery may be done by medial or anterior approaches.
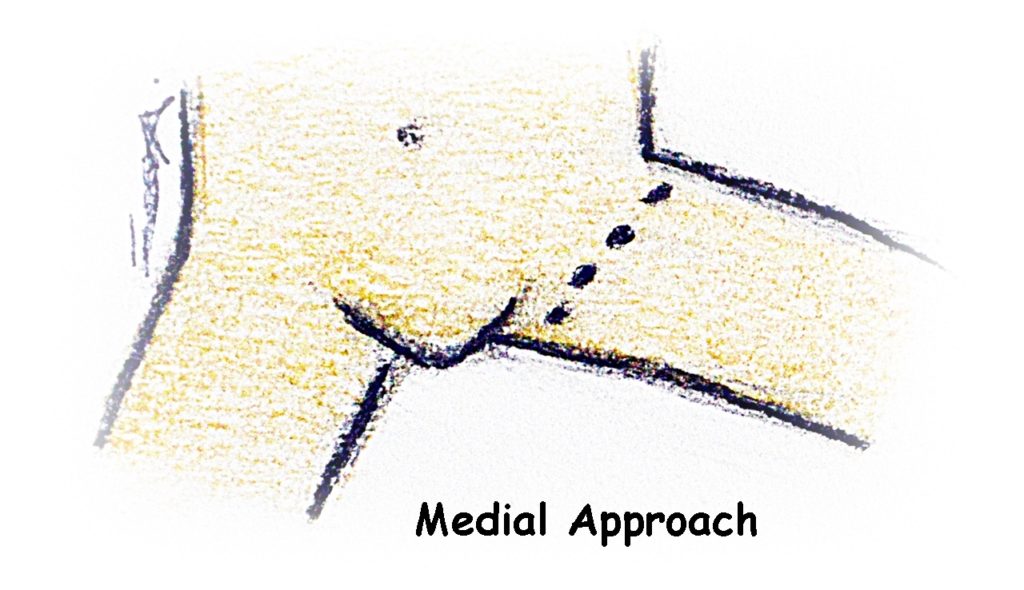
Medial approach:
Usually for children younger than 1 year; small incision in the groin; hip joint is cleared and femoral head is aligned into the acetabulum; use of hip Spica for few months.
Note: medial approach does not involve correction of bony structures.
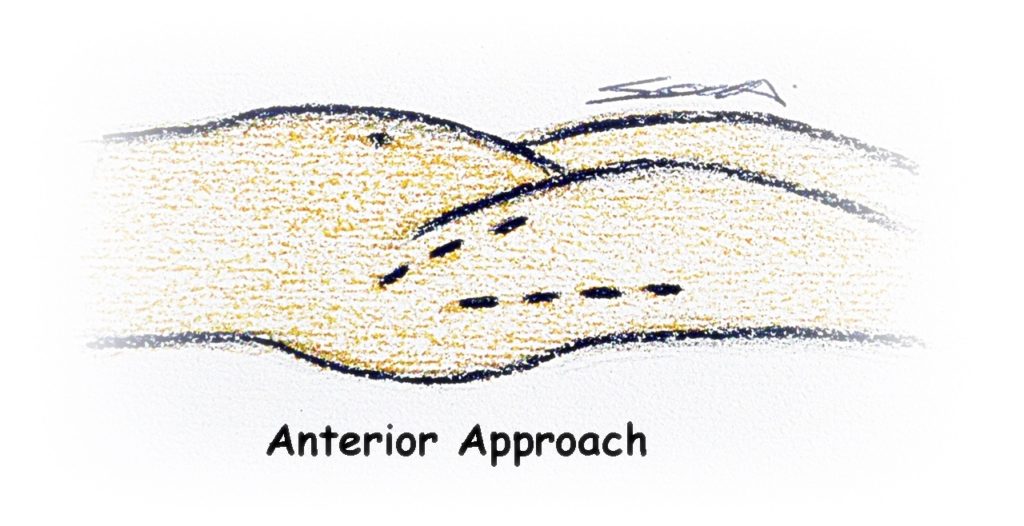
Anterior approach:
Usually for children older than 1 year; hip joint is cleared and femoral head is aligned into the acetabulum; ligaments around the hip are repaired and tightened.
Note: additional procedures to bony structures may be done using this approach, such as pelvic and femoral osteotomies.
E) Open reduction +/- pelvic osteotomy +/- Femoral osteotomy +/- casting – each surgical procedure may be done alone or combined; usually after 2 years of age the 3 procedures are performed; if pins and plates are used, another surgery will be needed to remove metalwork (a few months to 3 years later).
PELVIC OSTEOTOMIES: there are different types available to treat DDH. The choice is made upon on shape of the acetabulum and surgeon’s experience. Here are some examples.
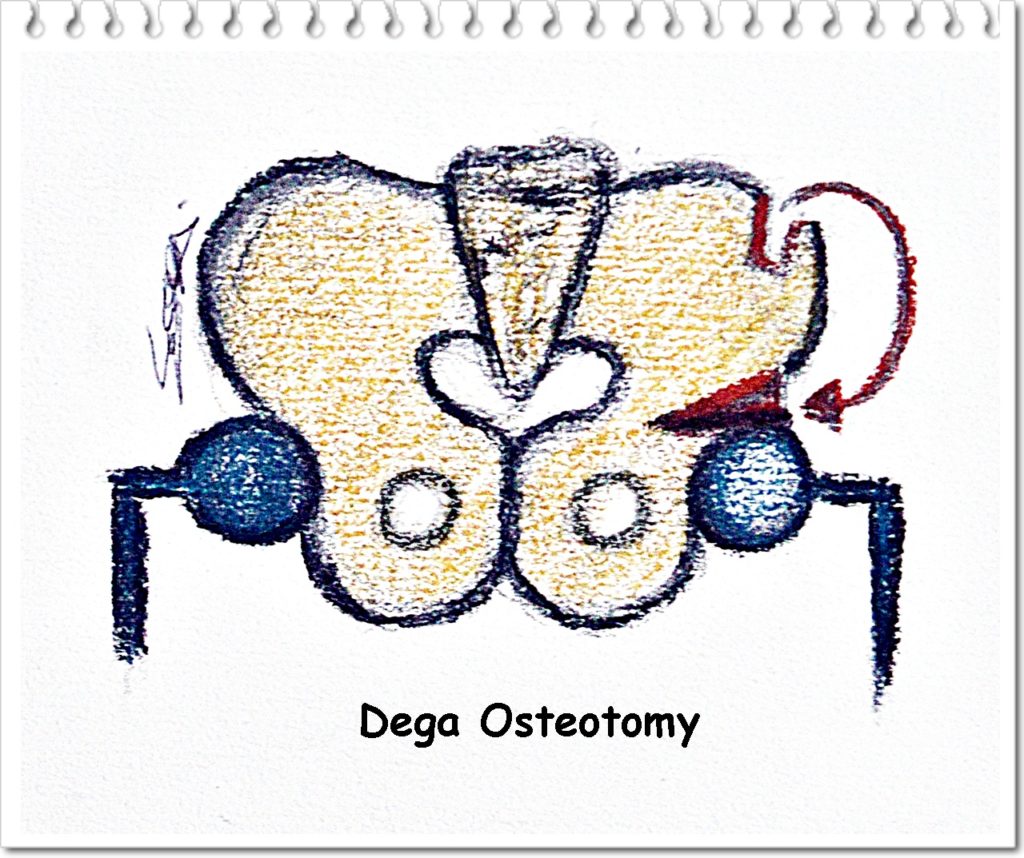
Dega osteotomy: when acetabulum is too wide and shallow.
(A) A two inch long incision is made in front of the pelvis;
(B) A surgical cut is made in the pelvis just above the acetabulum;
(C) The lower part of the pelvis is bent downwards to form a well-defined cup that covers the femoral head;
(D) The bone graft from A is placed over the space created by osteotomy from B.
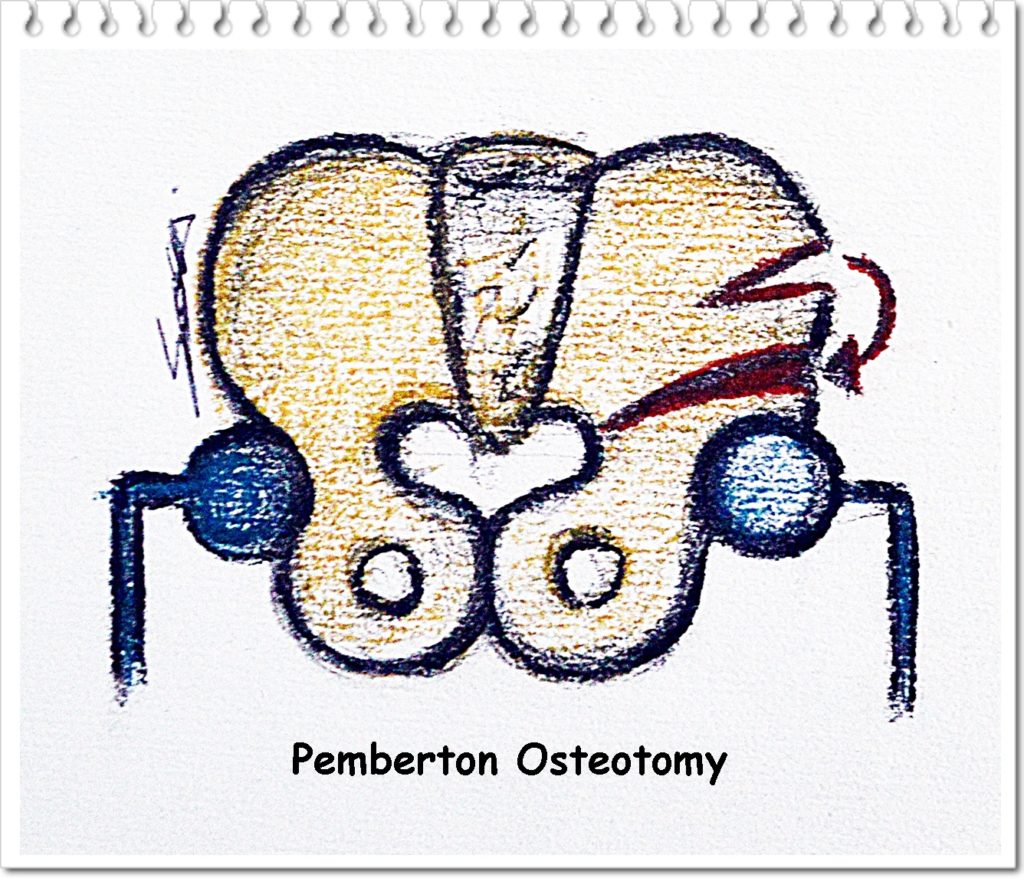
Pemberton osteotomy: when the acetabulum needs to be rotated down through the triradiate cartilage to change the direction and increase the depth of the socket.
(A) Osteotomy around the acetabulum is done (pericapsular osteotomy);
(B) Downward rotation of the acetabular cutting margins is performed to cover the femoral head;
(C) The corrected position of the acetabulum is maintained by inserting a bone graft taken from a wedge of the iliac crest.
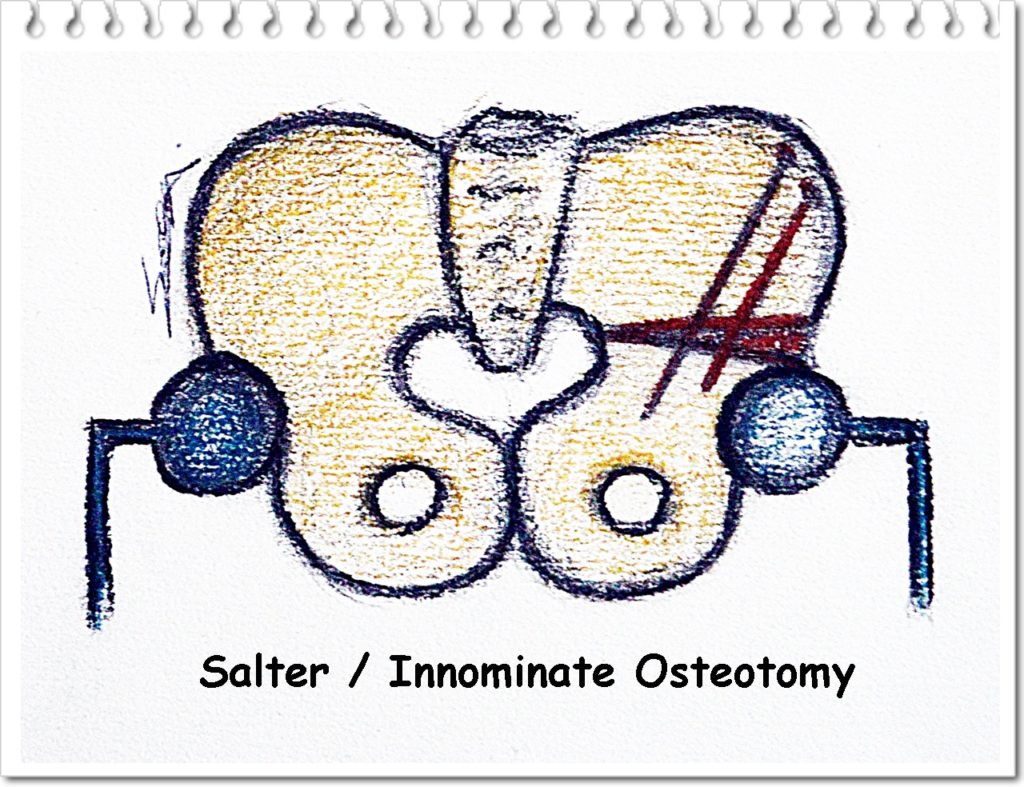
Salter/ Innominate osteotomy: when the acetabulum does not sit on top of the femoral head.
(A) Innominate bone osteotomy from the iliac bone right above the acetabulum is performed using a Gigli saw;
(B) Lateral rotation of the distal pelvic fragment is done for femoral head to be properly covered by the acetabulum;
(C) The corrected position of the acetabulum is maintained by inserting a wedge-shaped bone graft taken from the anterior iliac wing into the gap created by osteotomy from A;
(D) Threated wires are inserted to stabilize the acetabulum.
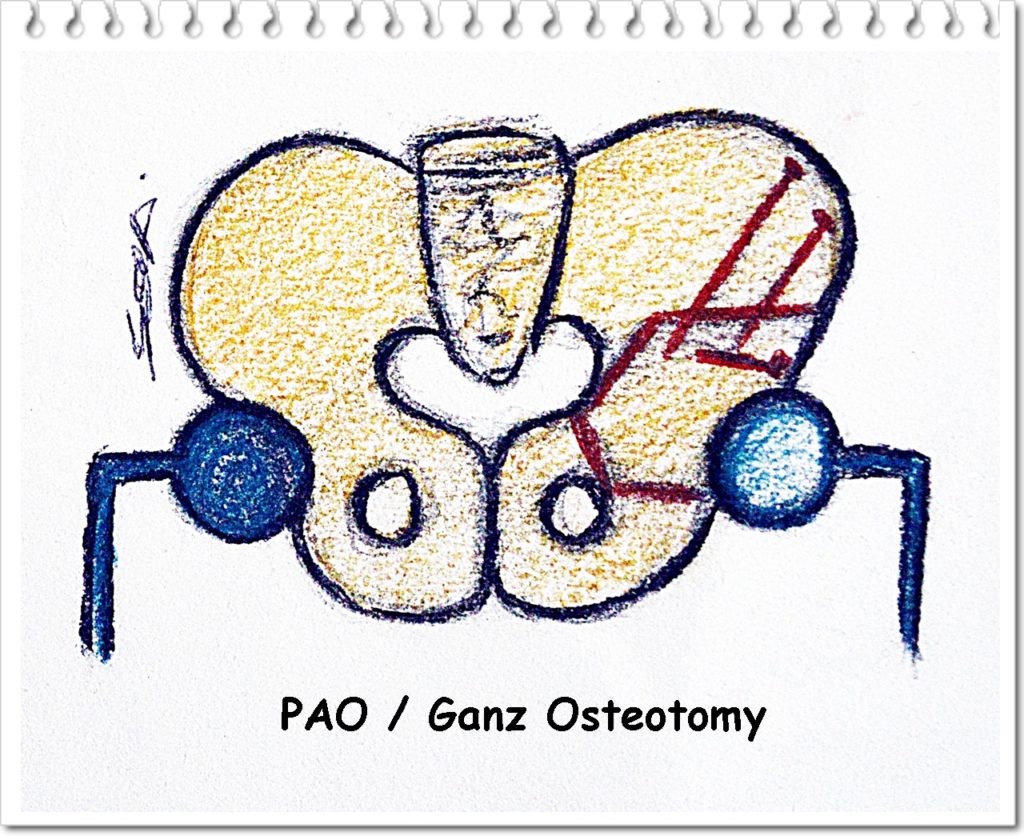
Periacetabular (PAO) or ganz osteotomy: when growth plate closure around the acetabulum occured, more common in adolescent and adults patients.
(A) A few osteotomies are made in the pelvic bone around the socket;
(B) The pelvic bone along with the hip socket is rotated to cover the femoral head in a correct position;
(C) To maintain that position, 2 or 3 small cortical screws are inserted.
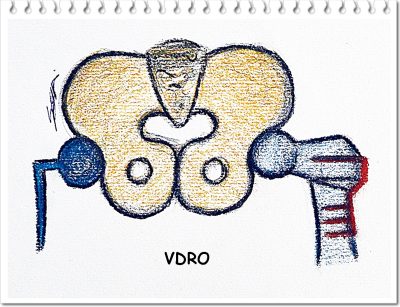
FEMORAL OSTEOTOMY: also called Varus osteotomy or Varus De-rotational Osteotomy (VDRO); when the femur needs to be angled in order to advance the femoral head further into the acetabulum.
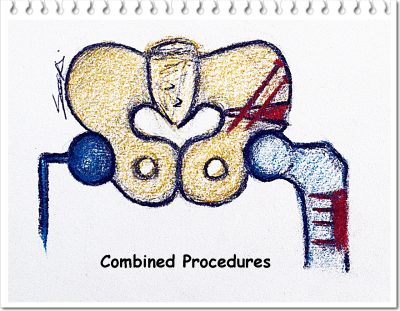
COMBINED PROCEDURES: involves Open Reduction, Pelvic Osteotomy, Femoral Shortening and Varus Osteotomy; involves surgical correction of all elements of hip dysplasia, requiring lesser time in the cast.