ECMO stands for ExtraCorporeal Membrane Oxygenation, also known as ExtraCorporeal Life Support (ECLS).
The aim of ECMO is not to treat the underlying patient’s condition, instead it provides the support for healing to occur. Additionally, ECMO can only help those with reversible lung and/or heart disease. Therefore, a careful decision about putting a patient into ECMO must be done (see Contraindications for ECMO more foward).
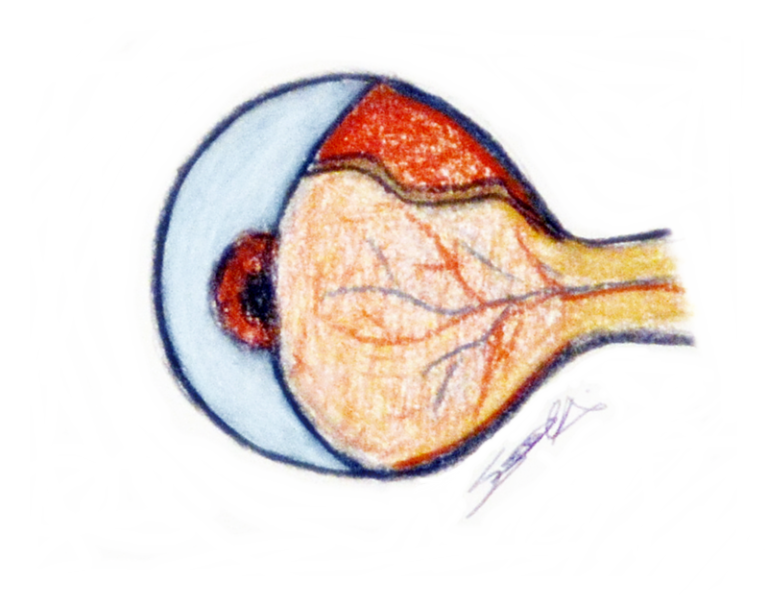
Before going into the principles of ECMO, it is necessary to understand how the Cardiovascular System works. Here is a simple diagram which explains the Pulmorary and the Systemic circulations.

ECMO machine and circuits
The ECMO machine basically pumps and oxygenates the patient’s blood outside the body, allowing the heart and lungs to rest.
BUT HOW? Once the patient is connected to an ECMO machine by air-free cannulas…
…The patient’s blood flows through the inflow cannula to a pump that pushes the blood to an oxygenator (artificial lung) where oxygen (O2) is added and dioxide carbon (CO2) is removed. The blood is then returned to the patient through the outflow cannula.
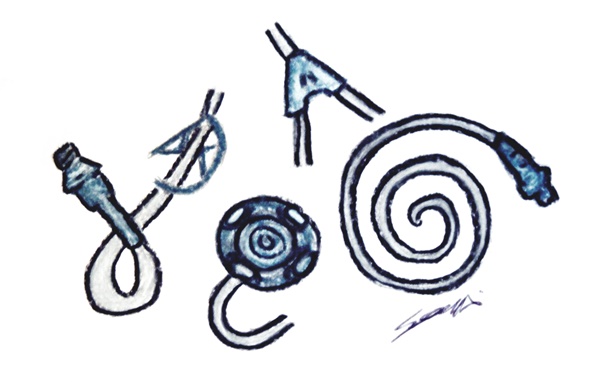
The 4 basic components of an ECMO circuit :
- Inflow/drainage cannula – it drains venous blood into the ECMO system; the blood in this cannula looks darker because it is very poor in oxygen;
- Pump – it moves the blood through the system;
- Oxygenator – a membrane system with analogous functions to the human lung, allowing gas exchanges (adds O2 and removes CO2);
- Outflow/return cannula – it returns newly oxygenated blood to patient’s systemic circulation.

Please note that depending on the situation, other components may be added to the circuit such as heat exchanger, monitors and alarms.
CRASH ECMO – The Emergency circuits must:
- be available within minutes of the call to a patient,
- be fully primed with crystalloid solution (type of volume expander for the circulatory system) and ready to attach as soon as cannulas are in place;
- include safety factors to avoid errors during emergent cannulation;
- include a microporous membrane lung (type of oxygenator) as it is easy to prime;
- include a high-pressure limited centrifugal pump, as it does not require monitors or alarms during initial set up.
There are 2 types of ECMO:
VA ECMO or veno-arterial ECMO: for patients requiring cardiac support or in cardio-respiratory failure; it provides both circulatory support and gas exchanges (ventilator functions);
VV ECMO or veno-veno ECMO: used for patients with respiratory failure; it only provides ventilator functions; there is no hemodynamic support, as the patient is dependent on his own hemodynamic physiology.
Next, attend the characteristics of each ECMO mode and the explanatory figures.

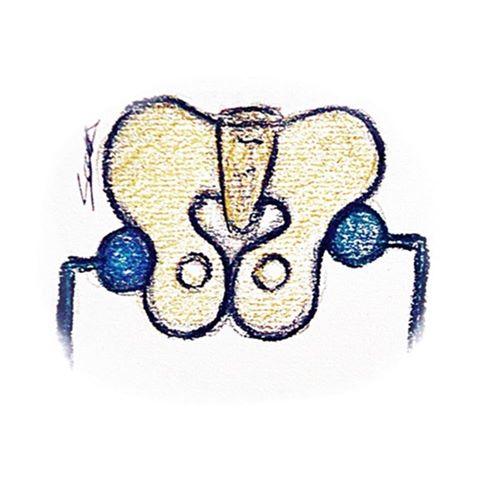
VA ECMO may be achieve by peripheral or central cannulation, in which an INFLOW cannula (drainage cannula) is inserted in a vein and an OUTFLOW cannula (return cannula) is inserted in an artery. The above diagram identifies the possible insertion sites of the cannulas as well as where their tips should rest (see parentheses).
For a better understanding, the below picture also identifies the possible places of INFLOW and OUTFLOW cannulas insertion in central and peripheral VA ECMO.


Note: The most traditional option for insertion of peripheral outflow cannula is the femoral artery, but axillary artery may also be used in adults, and the common carotid artery may be used in neonates or children with weight <15Kg.

In VV ECMO circuit the cannulas are placed only in the veins, and therefore there is a possibility to use only one cannula with double lumen (working as an INFLOW and OUTFLOW cannula) or use two different cannulas (an INFLOW cannula and an OUTFLOW cannula).


Note: This double lumen cannula is placed percutaneously into the right Internal Jugular vein, taking into consideration that one lumen drains deoxygenated blood from the SVC and IVC, and the other lumen returns oxygenated blood towards the tricuspid valve.

Cannulations approaches – The ECMO cannulas can be placed in 4 different ways:
- Cut down: exposure of the neck vessels; mostly performed in neonates and small children; usually done in the ICU with OR team; requires deep sedation/anesthesia and muscle relaxation to prevent spontaneous breathing and consequent air embolism;
- Percutaneously (Seldinger technique) by vessel puncture, guidewire and dilation; commonly used for VV ECMO in children over two years and in adults; may be performed in ICU, OR, or cath lab; the OR team is not essential but there should be a plan for direct cutdown access if there are complications with percutaneous placement;
- Cut down exposure and Seldinger cannulation: may be performed in the ICU, OR, or cath lab under anaesthesia; the vessel is exposed by cut down but not dissected, then, a seldinger technique by inerting catether, guidewire and cannula is used.
- Direct cannulation of the right atrium and aorta via thoracotomy/sternotomy; usually used for patients who cannot come off CardioPulmonar Bypass (CPB) in the OR, or in patients whose peripheral cannulation is not possible.
Main risks of ECMO:
- Bleeding: is the main risk during ECMO treatment; the administration of heparin to prevent clotting in the tubbing also increases the risk of bleading; the risk of bleeding increases when another surgical operation is required whilst patient is on ECMO;
- Infection at the cannulation sites entry;
- Clotting: to prevent clotting in the tubes heparin is administered;
- Embolism: before connecting the cannulas to the ECMO circuit, the surgeon must check for air bubbles in the tubbing to avoid embolism.
- Increased chance of stroke.
Contraindications:
Taken into account the risks of putting a patient in ECMO and that ECMO is a temporary support for the patient, it is important to consider the contraindications. Most contraindications are relative , which means that the decision to put a patient in ECMO must considered the risks of the procedure vs the potential benefits.
According to ElSO (2017) there are four main relative contraindications:
- Conditions incompatible with normal life if the patient recovers;
- Preexisting conditions which affect the quality of life (CNS status, end stage malignancy, risk of systemic bleeding with anticoagulation);
- Age and size of patient;
- Futility: patients who are too sick, have been on conventional therapy too long, or have a fatal diagnosis.
Acronyms used in this post:
CIA – Common Iliac Artery
CNS – Central Nervous System
ECMO – ExtraCorporeal Membrane Oxygenation
ECLS – ExtraCorporeal Life Support
IVC – Inferior Vena Cava
OR – Operating Room
SVC – Superior Vena Cava
References:
emblog.mayo.edu
gosh.nhs.uk
leicesterhospitals.nhs.uk
portal-chsj.min-saude.pt
bartshealth.nhs.uk
ucsfhealth.org
elso.org
academic.oup.com
aci.health.nsw.gov.au
annals.in
European Journal of Heart Failure
atm.amegroups.com
annals.in – article2
annalsthoracicsurgery.org – axillary artery VA ECMO
jtd.amegroups.com – important for ECMO diagrams