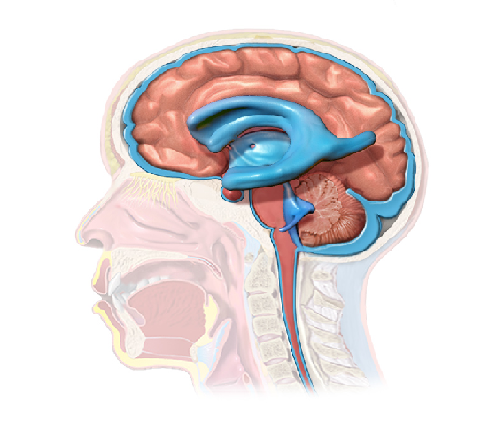
Tracheostomy is an artificial opening / incision through the neck into the trachea, usually between the 2nd and 4th tracheal rings, allowing the opening of the airway and helping the breathing.
This opening can be temporary or permanent, depending on patient’s condition. The procedure may be done:
- in operating room (by surgeons),
- at the patient’s bedside (widely performed on the Intensive Care Unit (ICU) by intensive care physicians using Percutaneous Tracheostomy approach)
- in emergency situations.
Anesthesia may be used before procedure. (note: during this post the surgical approach is discussed, but the rest of the information is also relevant for when performing Percutaneous Tracheostomy)
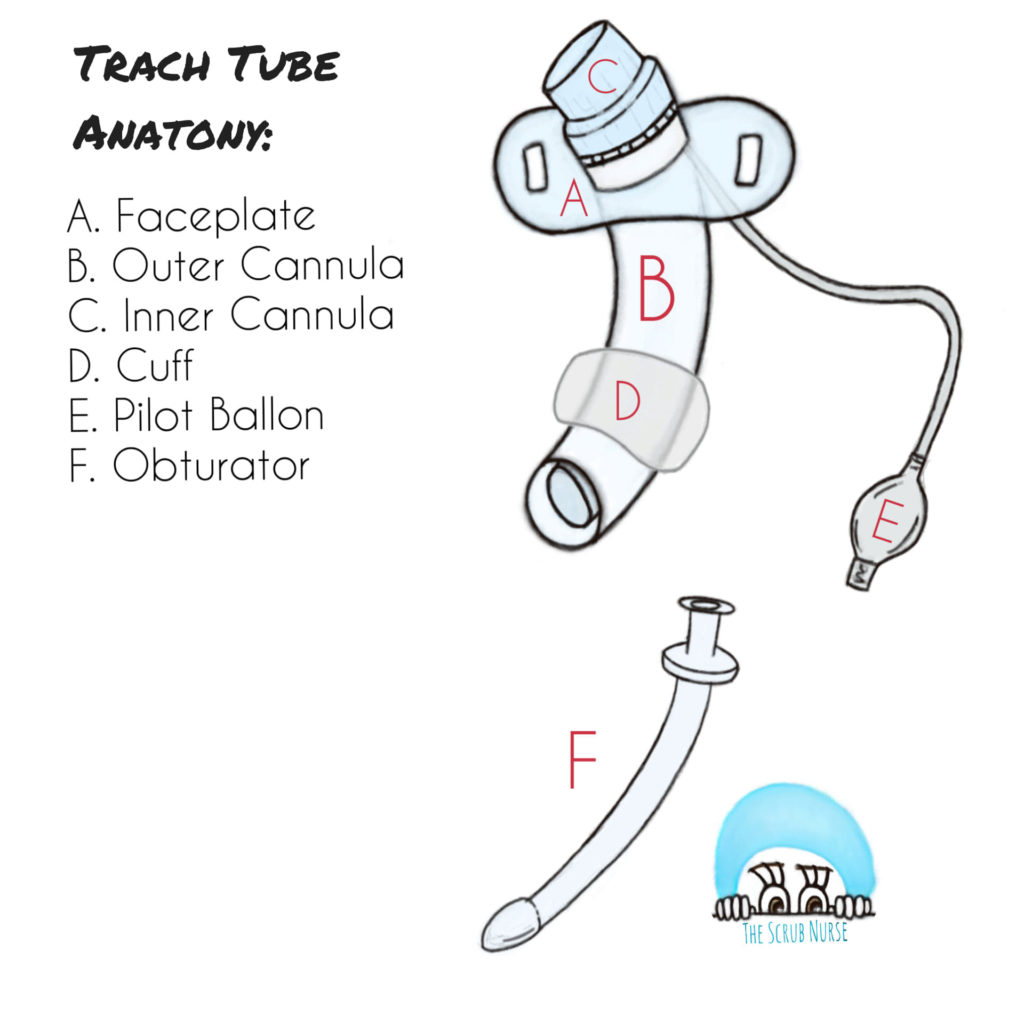
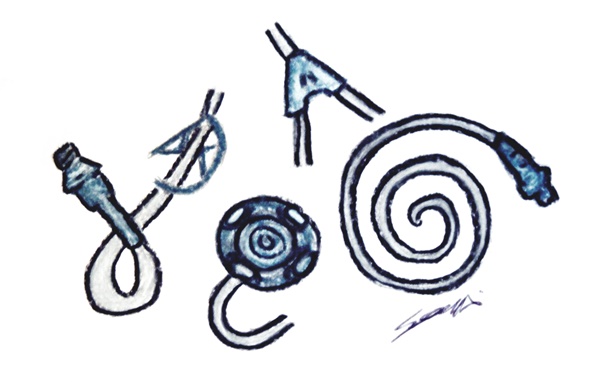
Anatomy of a Trach Tube
(A) Faceplate or neck flange – where the ties or sutures are connected to secure the tube in place; the type and dimensions of the tube are also indicated here.
(B) Outer Cannula – is the main body of the trach tube that is inserted into the trachea. Note: single cannula trach tubes only have this cannula, however dual cannula trach tubes also have an inner cannula.
(C) Inner Cannula – a cannula that sits inside the outer cannula and can be removed for cleaning purposes or if the tube is occluded, helping to manage the obstructions caused by secretions.
(D) Cuff – is present in some trach tubes to provide a seal (enabling positive pressure ventilation); to offer a limited protection to the airway from aspiration (if patient is vomiting); and to help control bleeding. Note: The pilot balloon (E) indicates whether or not there is air in the cuff.
(F) Obturator – also called “pilot”, is used to assist with the insertion of the tracheostomy tube and it has a blunt tip to avoid tissue damage. At this moment, the inner cannula is not in place, but after inserting the trach tube, the obturator is removed from the outer cannula and replaced by the inner cannula, if applicable.
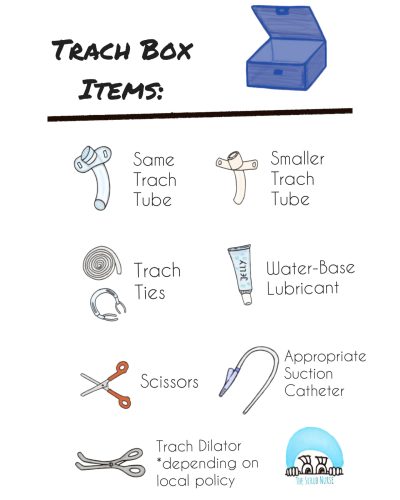
Emergency Tracheostomy Box
This box is designed to include the necessary equipment in case of accidental decannulation or for an emergency tube exchange. It should accompany the patient at all times and must contain ONLY the following:
- Spare trach tube (same size/make),
- Smaller trach tube (half size smaller – if paediatric; one size smaller – if adult);
- Suction catheter (appropriate size);
- Lubrication (water-based);
- Scissors (round-ended);
- Spare trach ties;
- Tracheal Dilator (depending on hospital policy – some institutions do not use)
Before inserting the tracheostomy, the surgical team must measure the suction length, to ensure that when suctioning, the tip of suction catheter must not protrude the end of the trach tube;
How to find the appropriate size of suction catheter? Some institutions use as a guidance the size of the trach tube and double it (e.g. size 3.5 trach tube = size 7 French gauge suction catheter).
In the other hand, Tracheostomy.org defends a guide created by Odell and others (1993):
(size trach tube – 2) x 2 = Appropriate French gauge suction catheter
(e.g. size 8 trach tube = 12 Fg suction catheter)
Whatever the used guide, the diameter of suction catheter should not be more than half of internal trach tube diameter, to allow patient to breath during suctioning procedure.
Note: Suction catheters that are too big may cause hypoxia during suctioning procedure, and those that are too small may not be effective in removing secretions.
A tracheostomy tube is held in place with trach ties around the neck, and this is fundamental to maintain safety airway.
The tapes must be tight enough to support the tube, considering that SHOULD NOT BE:
- too loose that the tube decannulates;
- too tight that there is excoriation of the surrounding skin
Trach ties tightening: It should only be possible to slip one finger comfortably between the ties and the patient’s neck.
The tracheostomy ties can be made of Velcro or Cotton; however the Velcro types are associated with higher rate of accidental decannulation, as they undo more easily, while the cotton types are hand-tied tapes.
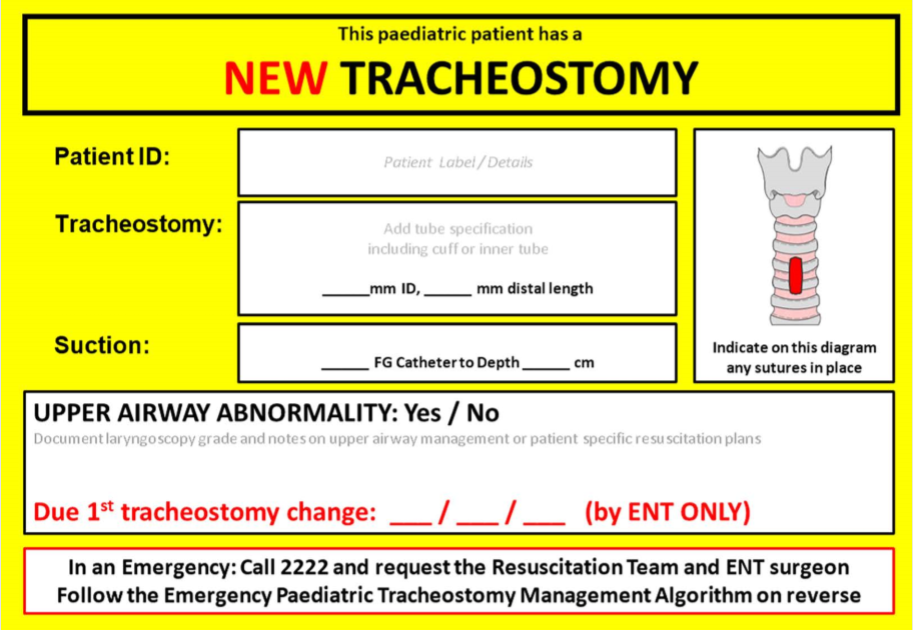
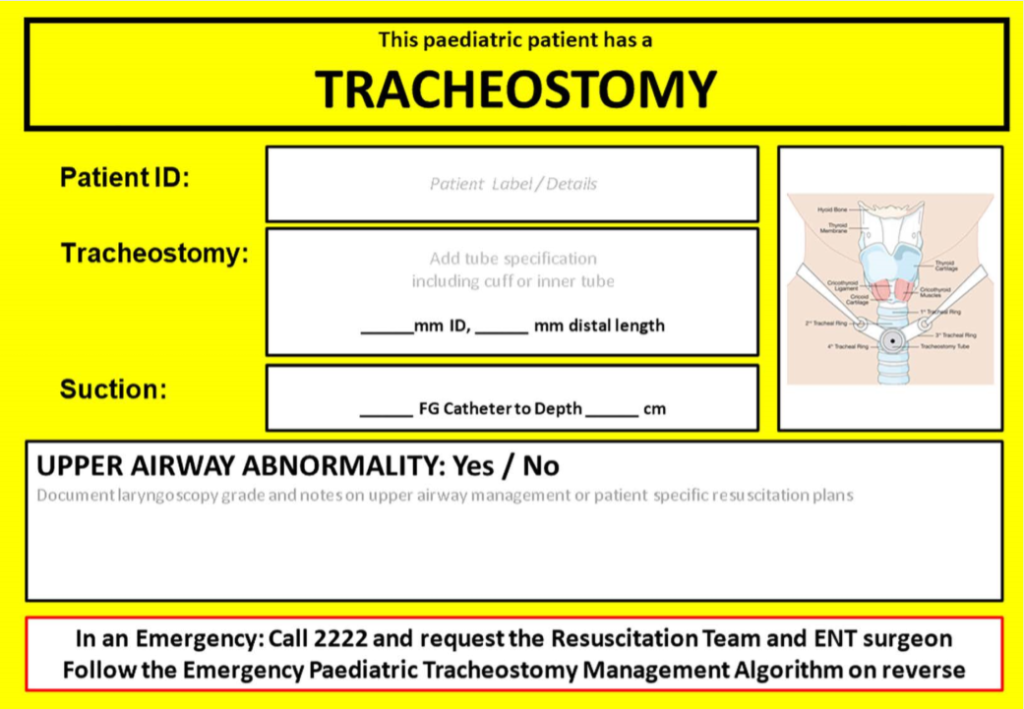
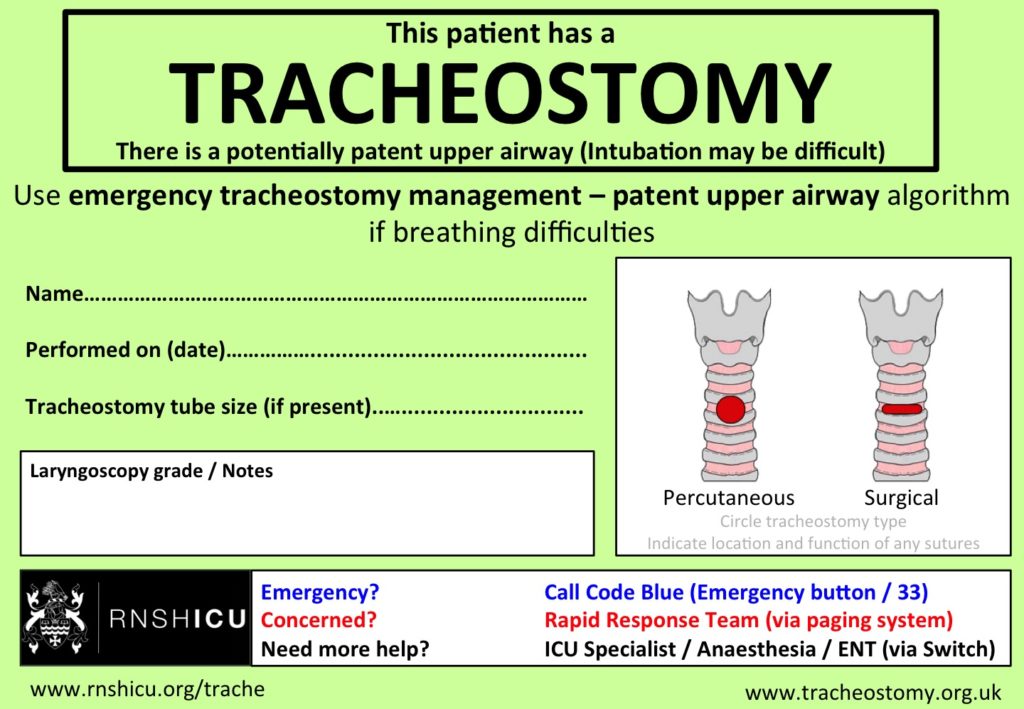
Tracheostomy Bed Head Signs
If a tracheostomy is performed in theatres, the theatre staff must send the card with the patients when sending them back to the ward.
How to perform a Tracheostomy (open approach)
See the videos below to have a better understanding of the step-by-step procedure.
Post-op Complications of Tracheostomy
Complications after inserting a tracheostomy might occur:
- Immediately: obstruction from sputum, blood clots or cuff; displacement of the tube; and haemorrhage
- After 36h: chest infection; wound infection; and mucosal ulceration
Emergency Care of a Patient with Tracheostomy
There are algorithms with step-by-step indications to follow in case of an emergency.
If paediatric patient click here: emergency paediatric tracheostomy management
If adult patient click here: patent airway algorithm – adult
References:
- GOSH - Tracheostomy care and management
- Tracheostomy Org - everything about Tracheostomies
- Cleveland Clinic - Tracheostomy Care
- Salisbury NHS Hospital - General principles and equipment required to safely manage a patient with a tracheostomy tube
- Trachs.com - Parts of a Trach tube
- Critical Care Airway Managment Course - Tracheostomy
- BJA - Percutaneous tracheostomy


Also you can do a tracheostomy at bedside electively. We do this routinely on adult ICU’s, called percutaneous tracheostomy’s
Yes that’s right! I added that info in the post to make it more complete and clear. I also added a link in references of an article from BJA that compares both surgical and percutaneous tracheostomies. However that won’t be discussed in this post (maybe in the future). Thank you
Suction catheter is the size of the traque tube x2 -2.
So for a traque size 8 it would be:
8×2-2
Size 14fr suction catheter
There wouldn’t be a point of using a size 4fr suction catheter on that case for example.
Dear ICU Nurse, during my research I found that the diameter of suction catheter should not be MORE THAN half of the internal diameter of the trach tube. I did found that Tracheostomy.org defends a guide proposed by Odell and others (1993) which says that (size of trach tube – 2) x 2 = correct French gauge of suction catheter. However I also found that other institutions have a different policy in practice, for example, the GOSH policies defend that the size of suction catheters is achieved by “double the internal diameter of the Tracheostomy tube (…) for example, a Tracheostomy tube size 4.0, use a suction catheter sized 8.0”. I do think that the appropriate suction catheter guidance might vary slightly, depending on institutions but the rationale is that while suctioning, the diameter of the catheter must not be too big that can cause hypoxia neither too narrow that it is not effective. However I will investigate more about it, and I will update here regarding this matter. Thank you for your comment and input 🙂