What is Spina Bifida?
A congenital condition developed during pregnancy, whose development of the baby’s spine does not occur properly.
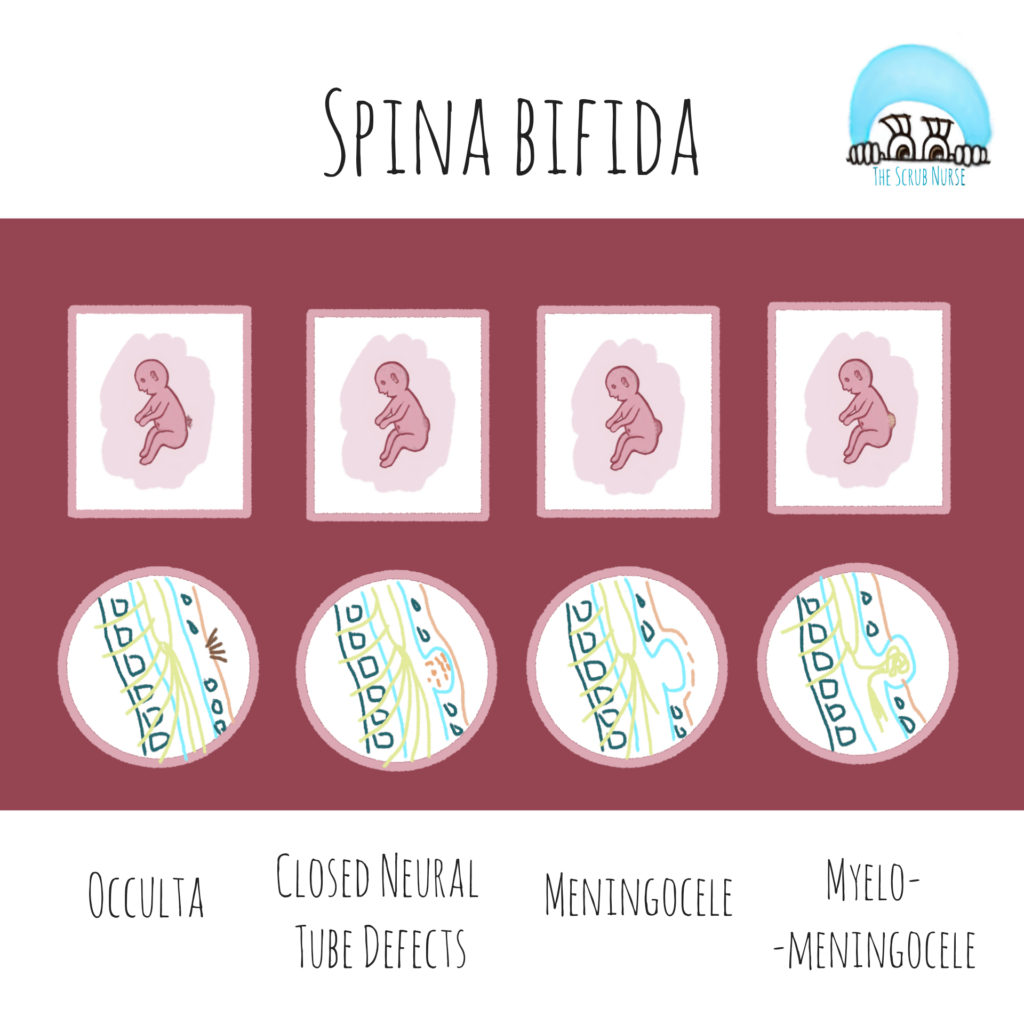
Spina bifica can be classified as an open or closed spina bifida, depending if the defect is covered or not by a skin layer.
There are 4 types of spina bifida:
- Spina Bifida Occulta,
- Closed Neural Tube Defects (such as lipomyelomeningocele),
- Meningocele,
- Myelomeningocele
The video below is an original of The Scrub Nurse, and it explains in a simple manner the differences between the 4 types of spina bifida.
Myelomeningocele (MMC) is the most severe form of spina bifida and generally, the extent of disability is related to the level of the myelomeningocele defect (usually higher upper level of lesion corresponds to greater deficits).
Common associated anomalies / disabilities are:
- hydrocephalus (needing ventriculoperitoneal shunt)
- motor and cognitive defects,
- bowel and bladder dysfunction,
- social and emotional challenges.
Fetal Surgery - A "heroic" intervention for MMC
Historically, fetal surgery is an operation reserved for severe fetal conditions in which intrauterine therapy may favorably alter a natural expected outcome, such as fetal/neonatal death or severe disability.
Laboratory and animal studies demonstrated that antenatal surgery for fetal MMC repair could improve neurologic outcomes.
Favorable results were attributed to:
- Less direct trauma to myelomeningocele while in utero,
- Less Cerebrospinal Fluid (CSF) leakage,
- Less exposure to amniotic fluid that is pottencially neurotoxic to the neurologic elements.
Fetal surgery for spina bifida is not a cure. However, since spinal cord injury occurs progressively during the gestation period, prenatal repair of myelomeningocele may prevent further damage.
Pre-Natal Repair vs Standard Postnatal Repair
Although prenatal repair may offer better results than traditional postnatal repair, open maternal-fetal surgery is a major procedure and carries risks to the mother and fetus. Those must be carefuly considered and they can occur at diverse stages – acutely, postoperatively, during pregnancy, and during subsequent pregnancies.
To assess the safety and efficacy of maternal-fetal surgery for the correction of myelomeningocele, in 2011, a Randomised Controlled Trial (A Randomized Trial of Prenatal versus Postnatal Repair of Myelomeningocele) conducted by MOMS investigators compared Pre-natal myelomeningocele repair with Standard postnatal repair. The main results of the study are identified below..
Advantages of Pre-Natal vs Post-Natal Repair
- Less deaths or cerebrospinal shunt requirement at 12 months of age (68% vs 98%)
- Less rate of hindbfrain herniation at 12 months of age (64% vs 96%)
- Double rate of independent walking at 30 months of age (42% vs 21%)
- Better neuromotor outcomes at 30 months of age
- More often, a better level of function than expected according to anatomical levels
Disadvantages of Pre-natal vs Post-natal Repair
-
More obstetric and maternal complications, such as:
- preterm birth <37 weeks (80% vs 15%)
- chorion–amnion separation (26% vs 0%)
- spontaneous membrane rupture (46% vs 8%)
- oligohydramnios (20.5% vs 3.8%)
- placental abruption (6.4% vs 0%)
- pulmonary edema (6.4% vs 0%)
- maternal transfusion at delivery (9% vs 1.3%)
- uterine thinning or dehiscence of the uterine scar at delivery (35.5% vs 0%)
- Long-term trial follow-up of both children and mothers (including subsequent pregnancy outcomes)
Another Studies:
- In 2014, a Cochrane review (Prenatal versus postnatal repair procedures for spina bifida for improving infant and maternal outcomes), concluded that high quality data comparing prenatal and postnatal myelomeningocele repair was limited to the single trial described above. And although it is a well-conducted study (with low risk of bias), it includes a small number of pregnancies, therefore firm conclusions can not be made. In addition, since the trial was conducted under rigorous settings, its results may represent only the best-case scenario and may not represent other cases that would be performed outside of the trial setting. In conclusion, this review concluded that there was insufficient evidence at the time to recommend intrauterine repair for spina bifida.
- In 2015, a most recent study (Fetal myelomeningocele: the post-MOMS experience at the Children’s Hospital of Philadelphia) published a single-center posttrial experience involving 100 cases of prenatal myelomeningocele repair. Short-term outcomes of Post-MOMS experience were comparable with results from original MOMS trial. Meaning that it is possible to achieve equivalent outcomes outside of the trial setting. However, because this study was performed at one of the primary centers that had participate in the original MOMS trial, there are limit conclusions regarding contemporary outcomes at nontrial centers that offer fetal MMC repair
Learn more about this innovative surgery - Fetal surgery
Children’s Hospital of Philadelphia (USA) were the pioneers of this operation. To understand better the pre-op preparation, the team involved and the steps of the surgery, please watch the following video about Prenatal repair of MMC, by Children’s Hospital of Philadelphia (available at https://youtu.be/qRtspxmhYnA).
The multidisciplinary team involved in the whole process is composed by:
- Fetal surgeons,
- Pediatric neurosurgeons,
- Fetal cardiologist,
- Obstetrician,
- Anesthesiologist (USA) / Anaesthetist (UK),
- Theatre nurses,
- Others such: maternal-fetal medicine specialists, neonatologists, sonographers, advanced practice nurses, a psychologist, social workers and coordinators
Prenatal myelomeningocele repair through open maternal-fetal surgery:
- Surgery is performed between 19 and 25 weeks’ gestation;
- Mother receives General anaesthesia (which also anesthetizes the fetus and relaxes the uterus);
- The fetal surgeon and pediatric neurosurgeon work together to perform the myelomeningocele repair similarly as they do on a newborn after birth.
1. The surgery starts with an incision in mother’s abdomen (laparotomy) and the uterus is exposed. A uterine stapling device is used to open the uterus (hysterotomy), it pinches the blood supply and keeps the membranes secured to the muscles) – performed by fetal surgeons;
2. Intraoperative ultrasound is performed to map the position of the placenta and the fetus, so the baby’s back can be rotated and placed in a way that the defect can be repaired – performed by maternal-fetal medicine specialist / pre-natal physician;
3. The defect is repaired by removing the MMC sac (if present), returning the spinal cord to the spinal canal, and closing the surrounding tissue and skin – performed by pediatric neurosurgeon;
4. The uterus and mother’s abdominal incision are then closed – performed by fetal surgeons.
The First time in London
Fetal MMC repair was recently performed for the first time in London by a team from Great Ormond Street Hospital (GOSH) and University College London Hospitals (UCLH). Please watch the folowing video that demonstrates in a simple way the step-by-step of this surgery (video by Great Ormond Street Hospital and Charity, available at https://youtu.be/QpNZInjNo3s).
Who is eligible for this surgery?
This surgical approach is very complex and available only to qualified candidates, demanding a team with experience to perform the surgery successfully and also a significant commitment on the part of mothers who choose to go forward with it.
References:
- ACOG – Committee Opinion about Maternal–Fetal Surgery for Myelomeningocele
- NEJM – A Randomized Trial of Prenatal versus Postnatal Repair of Myelomeningocele, MOMS Investigators
- Fetal Diagnosis and Therapy – Fetal Myelomeningocele Repair: The Post-MOMS Experience at the Children’s Hospital of Philadelphia
- Cochrane Library – Prenatal versus postnatal repair procedures for spina bifida for improving infant and maternal outcomes
- CHOP – About Fetal Surgery for Spina Bifida (Myelomeningocele)
- Mayo Clinic – Spina bifida
- Centers for Disease Control and Prevention – What is Spina Bifida?
- GOSH – First UK surgery in the womb for baby with spina bifida
- UCLH – UCLH offers fetal surgery for spina bifida for the first time in the UK
- Shine Charity – Types of Spina Bifida
- NINDS – Spina bifida fact sheet
- About Kids Health – Spina bifida
